When Pain Tells a Complex Story: Ruptured Endometriotic Cyst vs Appendiceal Pathology — A Diagnostic Journey
Hello Glias !
Acute lower abdominal pain in a reproductive-age woman often triggers suspicion of appendicitis. But sometimes, the real pathology lies within the ovaries — and can closely mimic gastrointestinal emergencies.
Here’s a recent case that emphasizes the importance of radiologic precision and multimodality imaging in diagnosing ruptured endometriotic cysts.
A woman presented with:
Severe lower abdominal tenderness
Pain radiating to the right lower rib
Guarding and rebound suggesting acute abdomen
Her ultrasound was challenging:
Appendix not visualized
Pelvic free fluid detected
No tubo-ovarian abscess (TOA) appearance
Previous history of hemorrhagic cyst under resolution
Differentials included:
✅ Ruptured hemorrhagic ovarian cyst
✅ Peritonitis from ruptured appendicitis
Given diagnostic uncertainty → Cross-sectional imaging warranted.
CT & MRI — Key Turning Point in Diagnosis
CT demonstrated:
Marked omental and pelvic fat stranding
Loculated pelvic fluid rather than diffuse ascites
Complex right multilocular ovarian cyst
MRI & TVS revealed:
Variable-age blood products within cyst
Absent sliding sign → pelvic adhesions
Deep infiltrating endometriosis at torus uterinus
→ Collectively pointing toward ruptured ovarian endometriotic cyst.
How Literature Supports Our Findings
| Feature | Seen in our case? | Supported by article? |
| ------------------------------------ | :---------------: | ------------------------------------------------------- |
| Multiloculated ovarian cyst |. ✅ | More common in ruptured endometriomas |Thick hyperdense cyst walls | ✅ | Thicker walls vs functional cysts (p < 0.05)
|Loculated ascites confined to pelvis | ✅ | Significantly more frequent in endometriomas
| Pelvic fat infiltration / stranding | ✅ | Suggestive of inflammatory reaction from rupture |
| Variable blood signal intensity | ✅ | Expected from repeated cyclic hemorrhage |
What We Ruled Out (and How)
| Condition | Why ruled out? |
| ------------------------- | -------------------------------------------------------------------------------------------- |
| Ruptured appendicitis| No peri-appendiceal epicenter of inflammation; appendix not thickened |
| TOA | No complex tubular mass, no pus-filled collection, no hyperemic adnexal inflammatory complex |
These distinctions are critical because:
Appendicitis → urgent surgical management
TOA → antibiotics + possible drainage
Endometrioma rupture → often conservative or laparoscopy depending on severity
Correct diagnosis reduces unnecessary invasive procedures.
Pathophysiology Refresher
Endometriomas rupture due to:
Increased intracystic pressure
Adhesion-related traction
Menstrual cycle hormonal changes
Spillage of degraded hemosiderin-rich content leads to:
✅ Severe chemical peritonitis
✅ Pain out of proportion
✅ Adhesions worsening endometriosis progression
This exact mechanism is emphasized in literature .
Final Diagnosis
Ruptured ovarian endometriotic cyst
with pelvic fat inflammatory reaction,
associated with deep infiltrating endometriosis,
without imaging evidence of appendicitis or TOA.
📚 Radiology Take-Home Messages
🔑 In women with acute pelvic pain:
Endometriosis should always be in differential
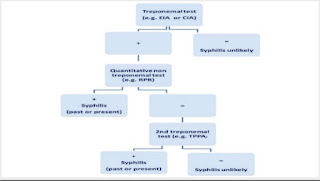
US may be nondiagnostic → CT/MRI are crucial next steps
Look for:
Multiloculated adnexal cysts
Thick walls
Hemoperitoneum but confined to pelvis
Pelvic fat stranding + adhesions
→ Highly suggest ruptured endometrioma.


Comments
Post a Comment